Our GP Dr Amun Kalia explains what it is, how it can be detected and what measures can be taken to improve bone health.
What is osteoporosis?
- Osteoporosis is a condition caused by low bone mass and deterioration of bone tissue. There is often an increase in bone fragility and subsequent susceptibility to fractures.
- Osteoporosis has no symptoms and often remains undiagnosed until an osteoporotic fragility fracture occurs.
- A fragility fracture is defined as a fracture following a fall normally from standing, although spinal fractures may occur spontaneously, or as a result of routine activities such as bending or lifting.
Causes of osteoporosis:
Osteoporosis is caused by an imbalance in the normal processing of bone remodelling. During normal ageing, bone is broken down by cells that eat bone, known as osteoclasts. When this process is increased and not balanced by new bone forming cells, known as osteoblasts, osteoporosis can occur.
The age when osteoporosis becomes apparent depends on:
- Peak bone mass, which is often reached in the third decade. It starts to decline in the fifth decade for men and women. In women, this decline accelerates after the menopause for a period of between 5 and 10 years. Peak bone mass is affected by genetic factors, but also levels of nutrition such as Vitamin D and calcium, sex hormone levels (testosterone and oestrogens), and levels of physical activity; in particular resistance exercise.
- The rate of bone loss, depends on a number of factors including oestrogen decline in women and a decrease in testosterone in older men.
Prevalence
Women are generally at greater risk of osteoporosis due to the decrease in oestrogen which occurs during the perimenopause and menopause. This accelerates bone loss in the peri-menopause and at a lower rate post menopausal. The prevalence of osteoporosis increases markedly, from approximately 2% at 50 years of age, to almost 50% at 80 years of age. In England and Wales, more than 2 million women have osteoporosis.
Osteoporotic fragility fractures:
- In England and Wales, around 180,000 of the fractures presenting each year are the result of osteoporosis.
- More than one in three women and one in five men will sustain one or more osteoporotic fracture in their lifetime.
- White men and women generally are at increased risk of fragility fracture compared with other ethnic groups.
- Vertebral fractures are often unrecognised and undiagnosed. Most of these tend to be osteoporotic fractures.
How do we assess our patients for fragility fracture risk?
We can offer a dual-energy X-ray absorptiometry (DEXA) scan to measure bone mineral density (BMD) depending on risk factors. This is routinely offered to our patients at risk as part of their annual health screening or arranged as part of a routine consultation. This is a painless scan carried out in a local hospital utilising X-Ray technology. Risk factors could include patients over the age of 50 with a history of fragility fracture. To help categorise risk, we can consider using an online risk calculator which helps predict the absolute risk of hip fracture and major osteoporotic fractures (spine, wrist, hip, or shoulder) over 10 years. In addition we can assess for vitamin D deficiency and inadequate calcium intake through a simple blood test. People are at risk of vitamin D deficiency if they are aged over 65 years, or are not exposed to much sunlight- which is the case for most of us who live in the UK! - A calcium intake of at least 1000 mg/day is recommended for people at increased risk of a fragility fracture.
What lifestyle information and advice do we give?
- Take regular exercise (tailored to each individual) to improve muscle strength.
- We encourage walking, especially outdoors, as this will increase exposure to sunlight, increasing vitamin D production.
- We encourage resistance or strength training, with weights if possible. A combination of exercise types, for example balance, flexibility, stretching, endurance, and progressive strengthening exercises is recommended.
- We encourage our patients to eat a healthy balanced diet as this may improve bone health.
- We always encourage smoking cessation if applicable, as it is a major risk factor for fragility fracture.
- We advise our patients to drink alcohol within recommended limits, as alcohol is another risk factor for fragility fracture.
What drug treatments do we recommend for our patients at high risk of osteoporotic fracture?
- Bone-sparing tablet medication can be prescribed in some cases by myself or one of my team.
- Other specialist treatment options include other oral medications normally prescribed through a consultant rheumatologist in severe or complicated cases.
- If our patient’s calcium intake is inadequate (<700 mg/day), we can prescribe prescription strength calcium supplements as well as prescription strength vitamin D for people who are not exposed to much sunlight.
- In addition we can consider prescribing hormone replacement therapy (HRT) to our younger perimenoposal and postmenopausal women to reduce the risk of fragility fractures and for the relief of menopausal symptoms given oestrogen remains a protective factor against osteoporotic fracture risk.
If you have further questions and would like to book in for a consultation, Dr Kalia and his team are available:
- Monday: 9am - 1pm
-
Thursday: 2pm - 6.30pm
- Friday: 2pm - 6pm
Our Barnes Clinic
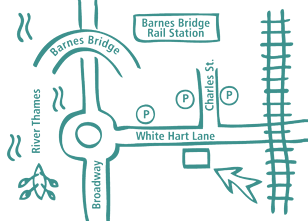
Our clinic is located in Barnes, South-West London and is easily accessible by public transport.
For more information including parking and other practicalities see our Barnes clinic page
Book an Appointment
Booking an appointment with one of our therapists is quick and easy. There is no long waiting time and you don’t need a referral from your GP.