By Christien, Matilda, Sharon and Michaela (Specialist Pelvic Health Physiotherapists)
Your Pelvic Floor – Why These Powerful Muscles Matter!
Pelvic floor health isn’t niche – it underpins your everyday wellbeing.
Why are pelvic floor muscles so important?
Your pelvic floor is a complex and responsive group of muscles supporting the bladder, bowel and uterus. These muscles play a vital role in:
• bladder and bowel control
• supporting the vagina and pelvic organs
• sexual function
• core stability and movement.
More than half of women will experience pelvic floor symptoms at some point, but these problems are not inevitable. Effective treatments exist, and early intervention can make a profound difference. Pelvic floor dysfunction can contribute to bladder and bowel symptoms, pelvic discomfort and changes in sexual function. These issues are common, yet they are not something you have to “just live with”.
Why train your pelvic floor?
Like any other major muscle group, the pelvic floor needs regular training. Weakness or poor coordination can affect your quality of life and become a barrier to physical activity. Strengthening these muscles can help you:
• improve continence and reduce leakage
• enhance support for the pelvic organs
• increase confidence and enjoyment during sexual activity
• optimise core stability for everyday movement and exercise
A helpful analogy: the boat in the dock.
To understand how the pelvic floor works, imagine a boat moored in a dock.
The ropes securing the boat are like the ligaments and fascia that support your organs. The water beneath the boat represents your pelvic floor muscles, absorbing and distributing load. If the water level drops, the boat drops and the strain on the ropes increases. When the water level rises, the strain is reduced. After childbirth or during hormonal changes, ligaments and connective tissue can stretch, but a strong pelvic floor can often compensate and protect the pelvic organs.
If pelvic floor muscle training alone doesn’t resolve prolapse or continence problems, other techniques and devices are available. For example, silicone pessaries can provide additional support for the bladder neck or vaginal walls. The most important thing is not to give up – help is available.
The evidence is clear: pelvic floor muscle training works!
Strong evidence shows that pelvic floor muscle training (PFMT) is one of the most effective first‑line treatments for urinary incontinence and pelvic organ prolapse in women of all ages. A well‑designed programme can improve:
• muscle strength and endurance
• coordination and relaxation
• blood flow to vaginal tissues
• lubrication and flexibility
• bladder, bowel and sexual function
Clinical trials demonstrate that it’s never too late to start.
Risk factors you may not expect:
Childbirth and hormonal changes are only part of the picture. Lifestyle factors such as:
• reduced physical activity
• changes in weight
• smoking
• chronic cough or constipation
can also increase symptoms. Because these are modifiable, addressing them offers a valuable opportunity for prevention and support.
Why women delay seeking help – and why they shouldn’t.
Bladder leakage is a major barrier to exercise, even though physical activity is essential for long‑term health. Research suggests that women who exercise are more likely to experience urinary leakage, yet many stop exercising rather than ask for help. When women are encouraged to talk about pelvic health, the response is often one of relief. Simple screening questions and early referral to a pelvic health specialist can be life‑changing.
Pelvic floor screening questions
Pelvic floor dysfunction is common and treatable. A pelvic health assessment is recommended if you answer “yes” to any of the following:
• Do you leak urine or faeces at any time?
• Do you struggle to control wind, particularly during exercise?
• Do you experience urgency or find it difficult to reach the toilet in time?
• Do you feel vaginal heaviness or notice a bulge?
• Do you experience pain during sex, tampon use, cycling or in daily life?
• Do you experience constipation?
• Do you have a persistent cough, wheeze or frequent sneezing?
• Have you had pelvic surgery or injury?
• Are you breast‑feeding?
• Are you perimenopausal or menopausal?
• Is your body mass index (BMI) over 25? (Higher BMI is associated with pelvic floor symptoms.)
If any of these resonate with you, remember that you’re not alone – and help is available.
Where to start
• The NHS‑endorsed Squeezy App is an excellent first step for guided pelvic floor training.
• If symptoms persist despite regular exercises, don’t give up. Book an appointment with our friendly and specialised pelvic health team: https://www.whitehartclinic.co.uk/treatments/womens-physio-south-west-lo....
Pelvic floor symptoms are common. Suffering in silence is unnecessary. Pelvic health physiotherapy works – and you deserve it.
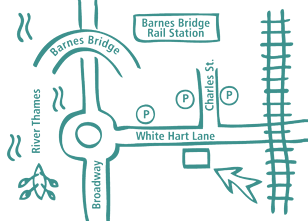
Our Barnes Clinic
Our clinic is located in Barnes, South-West London and is easily accessible by public transport.
For more information including parking and other practicalities see our Barnes clinic page
Book an Appointment
Booking an appointment with one of our therapists is quick and easy. There is no long waiting time and you don’t need a referral from your GP.