Achilles Tendinopathy can be an irritating and tricky injury to manage. Here we share some helpful insight on Achilles Tendinopathy; the condition, symptoms and how you might need to treat.
1.What is it?
The Achilles tendon is a continuation of the three calf muscles at the back of the leg that work to move the ankle. The tendon serves to connect these muscles into the heel bone and stores energy. It is continually loaded with running and walking.
Put simply, a tendinopathy is an inability of the tendon to deal with the load placed upon it. Many of the tissues in our body are in a constant state of breakdown and then renewal- not only is this necessary for life, but this allows us to get stronger and adapt to training. Our tissues (including tendons) respond to load, so how much stress we place upon our tendons dictates how much breakdown and then rebuilding occurs. Tendinopathies can occur not just in the Achilles tendon, but in other tendons throughout our body, just as the knee or shoulder.
If we place too much load on a tendon, and continue to repeat this process without allowing recovery, the amount of breakdown starts to exceed tendon synthesis- this causes a change in the structure of the particles that make up the tendon, which make it even more difficult for the tendon to deal with load.
2.What are the symptoms?
It is common in runners, but can also manifest in non-runners – often middle aged.
Sufferers often experience pain during or after a run or walk, and may be worse with stair or hill climbing.
The tendon may be painful to squeeze, and symptoms are often more noticeable upon waking or being stationary for a prolonged period. Many describe a “painful first few steps in the morning.”
3.Tendinopathy vs tendinitis
You may have heard the two terms used interchangeably, however there is an important distinction between these two terms. Previously, the condition was thought to be a result of inflammation, hence the suffix “itis” which denotes inflammation in medical terminology. We now know that the condition is in fact NOT inflammatory, and that changes such as swelling which may be seen are a result of changes in the tendon structure and not inflammatory cells. Hence, the term tendinopathy replaced the term tendinitis. This is crucial in understanding how to best treat the condition, as commonly used medications such as anti-inflammatories such as Voltarol may actually do more harm than good, depending on the stage of tendinopathy!
4. Location of Achilles tendinopathy
The tendon can be affected at one (or both) of two sites.
Insertional tendinopathy affects the tendon as it attaches into the calcaneous (heel bone). Mid-portion tendinopathy involves the tendon higher up, typically between 2 and 6cm from the heel bone.
It’s important to make this distinction as the two types are treated differently.
5.Stages of tendinopathy
There are three phases or stages of tendinopathy, however it’s important to remember these phases are a continuum rather than distinct phases.
Reactive tendinopathy is the tendons response to an increase in load- this may be increasing mileage, reducing rest days, or a change in intensity or training surface. In this stage, the tendon may appear swollen and be acutely painful. The good news is, the tendon remains structurally intact at this point and is it is usually a reversible process. It typically lasts 5-10 days, however the tendon will remain sensitive to load post this point.
Tendon disrepair
This follows the reactive stage if the tendon is loading beyond its capacity. The difference to the reactive stage is that the tendon shows structural changes.
Degenerative tendinopathy
The tendon structure is disorganised and less efficient at dealing with load. It typically appears thickened, and the risk of tendon rupture may be higher at this stage. It is more common in middle aged/older population. Unfortunately, some of the structural changes are not reversible at this point. This is not to say pain will be ongoing, however those with degenerative tendons need to be diligent with their physiotherapy and loading programmes to reverse structural breakdown that can be changed and allow return to activity.
To confuse matters, it is possible to have an acutely reactive tendinopathy on the background of a degenerative tendinopathy.
6. How long does it take to improve?
The news no one wants to hear! Unfortunately, if you’ve reached the degenerative phase, the tendon remodeling and return to loading process can take many months. Significant changes to your training will likely be necessary, such as cross training, rest days rather than recovery runs and reduction in sprint efforts and hill runs.
A biomechanical analysis of your running may also be of benefit to identify any other contributing factors to an overloaded tendon.
7. What should I do about it?
Don’t ignore it, tendinopathies rarely go away on their own. If you think you may be in the reactive stage, rest and seek the advice of a physiotherapist. During this stage, it is also best to avoid stretching (this is often debated amongst physiotherapists), however depending on which part of your tendon is involved, it may actually aggravate (this is often the case for insertional tendinopathy). Further, stretching the tendon places compressive load on it, so it may aggravate when in the reactive phase.
If you think you have a degenerative tendinopathy, a carefully constructed loading and training programme will be important:
- See your physiotherapist for an assessment and treatment programme tailored to you.
- Adjunct treatment modalities may also be recommended, including shockwave therapy which is offered at the White Hart Clinic. Our physios will assess and discuss a possible course of treatment if this the chosen route.
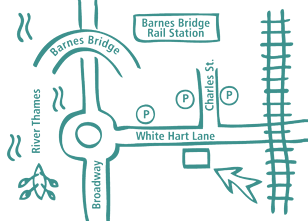
Our Barnes Clinic
Our clinic is located in Barnes, South-West London and is easily accessible by public transport.
For more information including parking and other practicalities see our Barnes clinic page
Book an Appointment
Booking an appointment with one of our therapists is quick and easy. There is no long waiting time and you don’t need a referral from your GP.